As a CTGR Member, Am I Eligible?
To qualify for PRC, you must meet the Federal requirements. In general, you must be screened by the PRC Staff for the following:
1. CTGR Tribal members must reside within the CTGR’s service area.
2. CTGR Tribal patients must complete the PRC application process.
a. CTGR Tribal members must provide documentation of their tribal enrollment status from the Confederated Tribes of the Goshute Reservation.
b. CTGR members must provide the proper documents for proof of residency.
3. CTGR Tribal patients must be enrolled in an alternative resource. Medicaid (Utah), Medicaid (Nevada), and Medicare must be utilized before seeking PRC support. The PRC Program is through Health and Human Services’ Indian Health Services and is considered by mandate to be the payor of last resort.

How to Become Eligible
· Step ONE: Complete the PRC Application
· Step TWO: Gather supporting documents.
- Tribal ID or CTGR Tribal Enrollment Document
- Identification Cards (driver’s license or State ID, and SS card)
- Copy of Primary Insurance Cards (front and back)
- Proof of Residency (Documents that support residency: Rental or Lease agreement, mortgage statement, utility bill, electric bill – issued within the last (60) days.)
You will be asked to be rescreened for the PRC program every 6 months or sooner. Proof of residency must be provided during the rescreening process. If you fail to provide the required documentation and do not complete the application process, (including follow-through with enrolling in an alternative resource), you will automatically be denied eligibility.
Exceptions to the Rule:
- CTGR Tribal eligible students who relocate outside of the CTGR PRC delivery area to attend school (full-time) may continue to access care paid for by the PRC program.
-
-
- Students must maintain a “full-time” course of study to keep their PRC eligibility status.
- Documentation will be required (per semester) to ensure continuous coverage outside of the CTGR delivery area.
-
- Minor children under the age of 19 in the household (natural or adopted child, stepchild, foster-child, legal ward, or orphan of eligible Tribal member).
- Non-CTGR Tribal women who are pregnant with an eligible CTGR Tribal member’s child who resides within the CTGR PRC delivery area during pregnancy through post-partum (6 weeks).
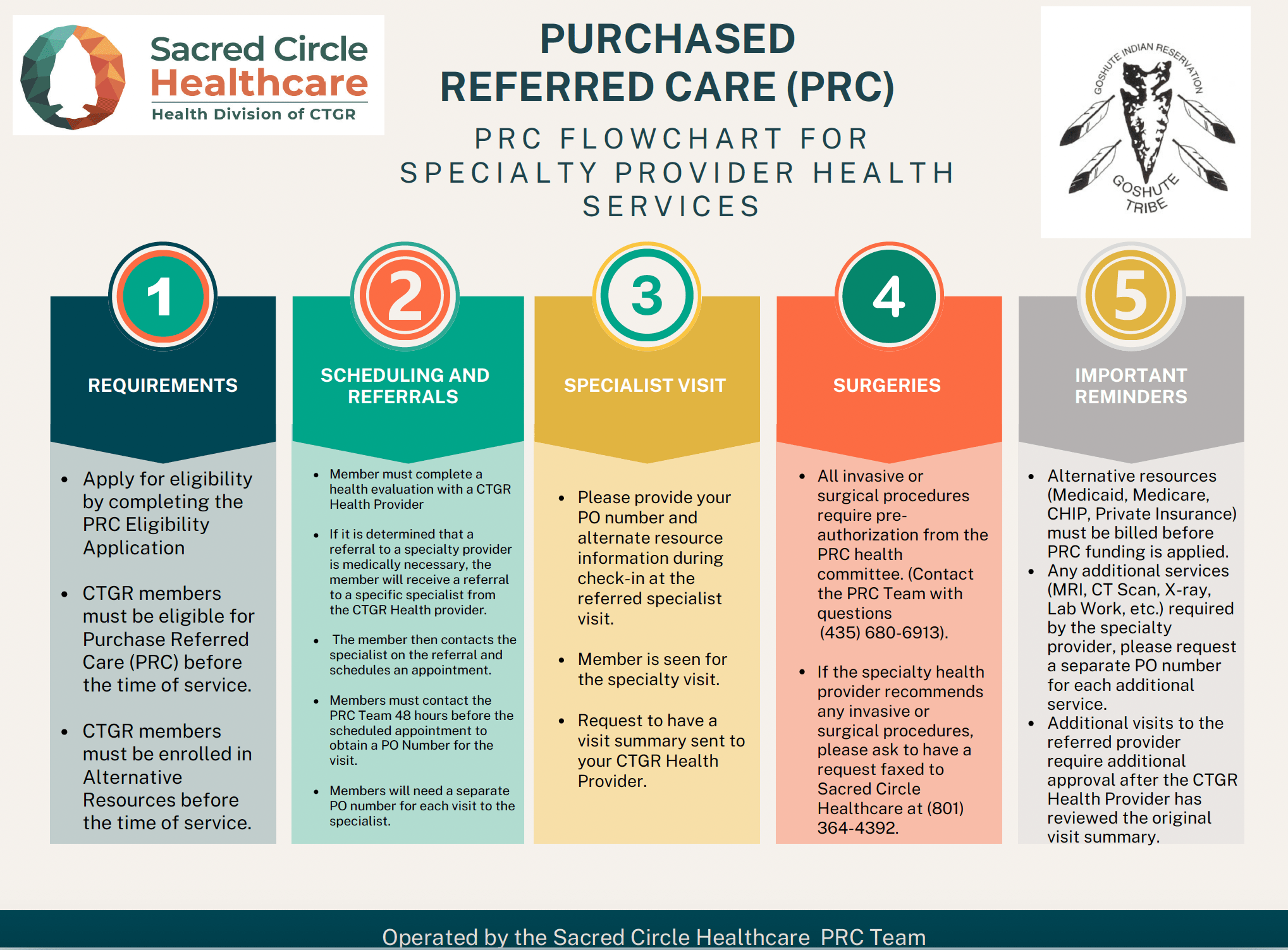
What is the Referral Process?
- CTGR Tribal patients must complete a health evaluation with a CTGR Health Provider
- Referral to a specialty provider is determined medically necessary.
- Once referred, the CTGR Tribal patient must verify their eligibility for the program with PRC staff.
- Purchase Orders must be obtained 48 hours in advance of the scheduled specialty visit (non-emergency).
- Pre-authorization is required for all non-emergency services and follow-up care.
- All emergency services must be reported to the PRC department within 72 hours after services have been provided (30 days for elders 55 years of age or older and disabled persons).
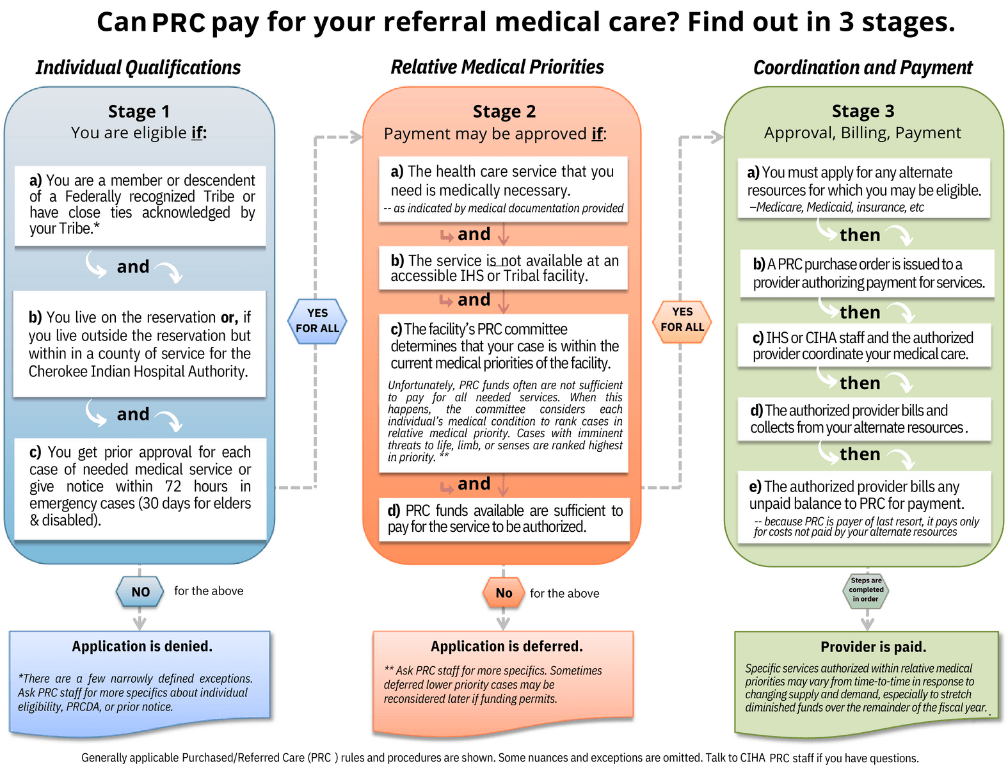
Common Reasons for Denial of PRC Coverage:
- Eligibility
- The patient failed to obtain prior approval from the PRC department for non-emergency services.
- The patient failed to notify the PRC department within 72 hours (or 30 days for elders 55 years of age or older and disabled persons) after seeking emergency services.
- Services not within the medical priority level care funds
- Services being denied from alternate resources (i.e., private insurance, state Medicaid, Medicare, etc.) due to failure to complete patient responsibility.
- Patients who refuse to use alternate resources or be screened for alternate resources.
